EHCR: An EU Provenance Case Study
Introduction
Cooperation among people using electronic information and techniques is an
increasingly common practice in every field, including healthcare applications.
In the case of distributed medical applications, the data (containing the
healthcare history of a single patient), the workflow (of the procedures carried
out on that patient) and the logs (recording meaningful events in those
procedures) are distributed among several heterogeneous and autonomous
information systems. These information systems are under the authority of
different healthcare actors such as general practitioners, hospitals, hospital
departments, etc. which form disconnected islands of information.
The distributed nature of healthcare institutions sometimes hinders the
treatment of patients, because documentation of the healthcare history and
therapy of a patient is split into independent healthcare institutions. In order
to provide better, user-centered healthcare services, the treatment of a patient
requires viewing the processes and data as a whole. Although agent-based
cooperation techniques and standardized electronic healthcare record exchange
techniques support the semantic interoperation between healthcare providers, we
still face the problem of the reunification of the different pieces of the
therapy of a single patient executed at different places. Currently there are
some countries that have no unification method for patient healthcare records;
each region in the country or even each institution inside a region may have its
own medical record system, sometimes not even fully electronic, and with no
automatic health care record exchange mechanisms. Therefore, it is not uncommon
for doctors to depend on the patients themselves in order to include data from
previous treatments and tests.
Making electronic systems provenance aware enables users to trace how a
particular result has been arrived at by identifying the individual and
aggregated services that produced a particular output. In healthcare systems
there is a need to provide an integrated view of the execution of treatment
processes, to analyze the performance of distributed healthcare services, and to
be able to carry out audits of the system to assess that, for a given patient,
the proper decisions were made and the proper procedures were followed. All of
these tasks depend on being able to trace back the origins of decisions and
processes, the information that was available at each step, and where that
information came from. Note that the provenance of a piece of data is primarily
about the causal dependencies of execution steps, although time sequences can
also be handled. The provenance architecture of focuses on making
service-oriented systems provenance aware, but making healthcare systems
provenance aware needs additional techniques, because healthcare actors are
autonomous and, unlike in service oriented systems, they may participate in the
same process without directly interacting with each other.
Overview of Application
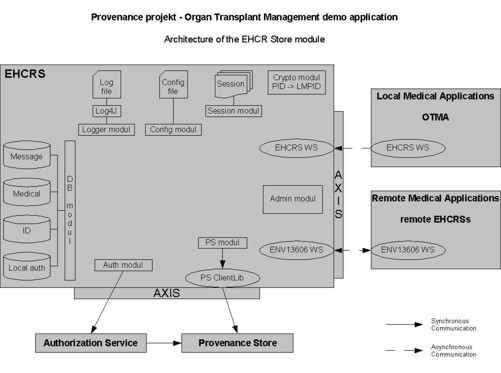
The EHCR architecture implemented by the
System Development Department of
SZTAKI provides a way to build electronic
health records as well as a unified view of a patientís medical record. The
architecture provides the structures to build a part of or the full patientís
healthcare record drawn from any number of heterogeneous databases systems in
order to exchange it with other healthcare information systems. It uses the
ENV13606 pre-standard, which defines the messages, the retrievable objects, the
healthcare agents and the distribution rules.
Current healthcare systems in many countries work by storing master copies
data about individual medical treatments on a patient at the place where the
treatments are carried out. Most commonly a single GP oversees a patientís
medical history and thus integrates treatments not carried out under his/her own
supervision post event. However there is no standard process for forwarding
medical details which might form part of the record to a central registry or a
master copy a particular patient's record. Information is retrieved from
different healthcare providers on the basis of the patients Identity Number
(ID). A healthcare provider A may only ask for record information from another
provider B for a patient X if the patient X is physically being treated at A.
Usually there is no central health authority database that could be relied upon
to have a complete medical history.
In order to pull together the medical history of a patient we have
essentially three options:
-
Build a system mirroring the current one based on fragments of records
in different places which can be pulled together to produce a unified view
on demand (depending on the permissions of the viewer).
Build a system of a more centralised nature with a master record which
can be read and written to by authorised healthcare providers (in a
controlled fashion) and possible cached at a particular healthcare provider.
Build a hybrid system which stores fragments of data with providers but
records high level events in a central master record.
In all cases the interchange protocol could be one of the European
pre-standards. Our approach follows the third option above.
Security Issues
When we extend healthcare systems with provenance in order to provide better
services for patients, then we face new privacy issues in addition to those
already handled in the healthcare information system.
Organizational and technical measures help to protect the privacy of the
patients in usual healthcare information systems. In these systems the patient
and the medical data are stored in EHCR management systems and transmitted
between these systems. The separation of data and the different kinds of access
control techniques protect the identity of the patient. The anonymity of medical
data allows controlled and irreversible disclosure for different purposes
mentioned earlier. In these systems the data is completely under the control of
the actors comprising the distributed system and data sharing is controlled by
the agents.
When we want to increase trust in data and to increase the quality of medical
services in distributed medical applications by introducing provenance concepts,
we introduce new privacy risks as well. We introduce the provenance store into
the systems. In order to be able to trace how a particular result has been
arrived at by identifying the individual and aggregated services that produced a
particular output, the actors of the system must entrust information to the
provenance store. This way healthcare actors give up part of the control over
the data and the autonomy of the healthcare information is shared with the
provenance store which is then able to link data and the workflow pieces that
generated the data.
One of the problems of healthcare information systems is that there are
information islands. While the healthcare data exchange standards help the
information exchange between these islands, the provenance system helps the
integration of the islands. This raises additional privacy risks.
The purpose of using a provenance system in the healthcare applications is to be
able to trace back the processes that happened whenever an audit is needed to
verify, e.g., the chain of decisions made for each case, or the compliance of a
treatment with respect to the related regulations. However there may be a
conflict between provenance and privacy. While for provenance we need as much
information as possible about the whole process (who did what and when) to be
able to trace back all that has happened, for privacy we need to restrict as
much as possible the information available in order to avoid identification of
patients and practitioners by unauthorised users.
The use of distributed provenance stores to register all relevant information
in a distributed medical information system poses two main risks:
cross-link risk: the risk that unauthorised users are able to link some
piece of medical data with an identifiable person by cross-linking
information from different sources.
event trail risk: the risk to be able to identify a person by connecting
the events and actions related to that person (e.g., the hospitals he has
visited in different countries).
Process Documentation
We introduced two techniques to reduce the cross-link risk: a) we do not put
medical data in the provenance store that can be easily used to identify the
patient, and b) we anonymise the patient data.
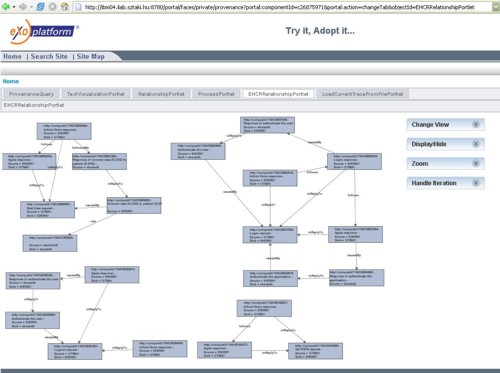
When mapping the provenance architecture to the OTM application, we decided
not to store sensitive medical data in the provenance store, but only references
to such data. This way the provenance store contains only the linkage and the
skeleton of the provenance of the medical data, and the healthcare data can be
laid on the skeleton by retrieving it from the healthcare information system
when needed. The retrieval is done by an EHCR system which is completely under
the control of EHCR access rules. With this approach we keep the same privacy
degree of medical data as in the original system. Moreover we also minimalise
the amount of transferred data.
One might think that if we do not store medical information about patients in
the provenance store, then there is no need to anonymise the patients and we can
use real patient identifiers in the provenance store, because no medical
information can be inferred on the patient. However this is not the case. Even
the fact that the patient was treated, can be sensitive information, because it
may increase the event-trail risk mentioned in the previous section, and also
because the reference to the place where the medical data of the treatment was
carried out may refer to the type of treatment the patient received. The type of
institution can reveal the type of medical intervention for example because if
the institution is specialised on heart diseases, then the reference to this
institution reveals that the patient was treated with heart problems. Therefore
at least the patient identity has to be anonymised.
The anonymisation process has to satisfy two requirements as described in the
following. In order to be able to create a complete and interlinked process
documentation of the treatment of the patient, if two sets of p-assertions are
related to the same patient, then there should be a way to link anonymised
patient identifiers referring to the same patient in the different sets of
p-assertions. In order to protect the privacy of the patient, the anonymisation
procedure should be irreversible in the sense that nobody should be able to tell
the real identity of the patient by knowing the anonymised identifier in the
provenance store. As a consequence of this, no component in the system should
store the real identifier of the patient and its anonymised identifier together.
In the OTM application, the EHCR subsystem applies case identifiers (identifiers
created at run-time) as tracers to make connections between sets of
p-assertions. The case identifier is anonymous, because it does not contain the
identity of the patient. Using this identifier in the provenance store is
similar to the anonymisation method of EHCR systems and yields similar privacy
degree within the provenance documentation of one case.
When we want to connect different cases, we have two choices: a) we store two
or more case identifiers in any of the p-assertions and define relationships
between the case identifiers, or b) we use a global anonymous tracer of the
patient and connect each case identifier to that anonymous tracer in
p-assertions. The first solution corresponds to the current practice where the
doctor knows (for example from the patient) that the current case is related to
a previous one. In this case the doctor connects the cases with a relationship
p-assertion in an ad-hoc way, therefore it is not recommended. The second
solution helps to connect those cases as well, that are not explicitly known,
therefore we followed this approach.
In the second solution we send the case identifier and the public identifier
of the patient to an authorisation agent who is responsible for all
authorisations in our systems. The authorisation agent generates from the public
identifier of the patient (such as national insurance number) an anonymous
tracer, called Global Medical Patient Identifier (GMPID ) and makes a
p-assertion in the provenance store connecting the case identifier with the
GMPID. This way all case identifiers, which are about the same patient, will be
connected to the GMPID of the patient in the provenance store. When we query the
p-assertions that relate to the same patient, we can use any of the case
identifiers, because case identifiers related to the same patient are linked
together. This way the authorisation agent connects the different identity
domains together.
When we want to retrieve the medical history of the patient, then we ask from
the provenance store where and when the patient was treated, and then we have to
query all the other medical information directly from the hospitals where the
patient was treated because they are not stored in the provenance store.
Advantages of Provenance Aware EHCR Systems
In addition to the ability to return the whole process documentation, the
method described above has two other advantages as well. One is that the actors
can improve the quality of the process documentation and the other is that they
can improve the quality of their own activities.
The quality of the process documentation can be improved if the actors
discover some relationship from the real processes (e.g. the current illness of
the patient is a consequence of a problem in the previous treatment not
discovered before) then they can improve the process documentation by augmenting
the already existing naming service based links with the direct causal
relationships present in the process. This is now possible, because the
p-assertions relevant to a single object can be located and linked to following
the links.
The actors can improve the quality of their own activities using the linked
process documentation, because when an actor executes its treatment process, it
can already retrieve the p-assertions of other actors and might be able to
discover a relationship from the provenance information. For example if the
physician knows the details of the previous treatment of the patient, then
he/she might use that information in the current treatment.
