Applying Provenance in Organ Transplant Management
Treatment of patients through the transplantation of organs or tissue is one
of the most complex distributed medical processes currently carried out. This
complexity arises not only from the difficulty of the surgery itself but also
from a wide range of associated processes, rules and decision making which accompany
any transplantation case. Depending on the country where a particular transplant
is being carried out procedures and the level of electronic automation of information
/ decision making may vary significantly. However, it is recognized worldwide
that ICT solutions which increase the speed and accuracy of decision making
can have a very significant positive impact on patient care outcomes.
The Organ Transplant Management (OTM) Application aims to
speed up the allocation process of solid organs to improve graft survival rates.
Its policy implements the Spanish guidelines for organ and tissue procurement
and Spanish regulations for allocation, as Spain is world leader in the area,and
its model is followed by other countries. OTM uses standard web service technology
and has been adapted to be provenance-aware, by interacting with the provenance
stores in order to keep track of the distributed execution of the allocation
process for audit purposes.
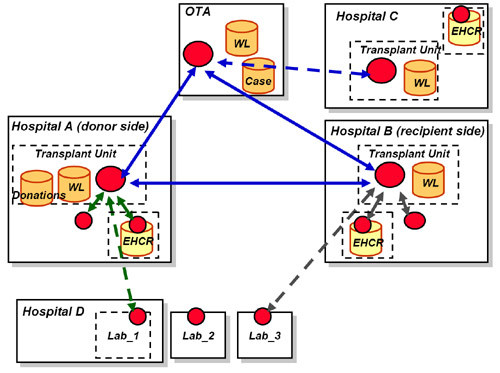
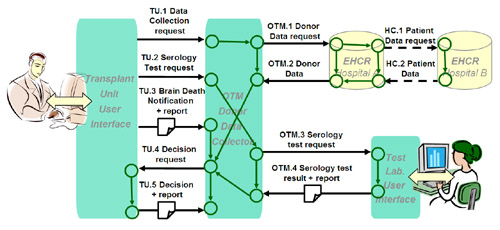
The diagram above summarizes the different administrative domains (solid boxes)
and units (dashed boxes) that are modelled in the OTM application. Each of these
interact with each other through Web Service interfaces (circles) that send
or receive messages. The Regional or National Organ Transplant Authority (OTA)
is an administrative domain with no internal units. In a transplantation management
scenario, one or more hospital units may be involved: the hospital transplant
unit, one or several units that provide laboratory tests and the unit that is
responsible for the patient records (which will use the EHCR application services.
The diagram also shows some of the data stores that are involved: apart of the
patient records, these include stores for the transplant units and the OTA recipient
waiting lists (WL). Hospitals that are the origin of a donation also keep records
of the donations performed, while hospitals that are re-cipients of the donation
may include such information in the recipient's patient record. The OTA has
its own records of each donation, stored case by case.
The OTM application was modeled in conjunction with the Spanish National Government
FIS Carrel project, a project carried out jointly between Hospital St. Pau i
Santa Creu and UPC in Barcelona Spain. It has been developed in Java 1.5 and
the modular components are deployed as web services. The user interface of the
OTM Application is the OTM GUI, a web application developed in Java 1.5 using
the Google Web Toolkit. This application serves DHTML web pages that allow the
user to interact with the OTM components representing the user's organizational
unit.
Overview of the Organ Transplant Management Scenario
An organ transplant case management is a distributed medical process where
decisions are taken by different actors in different institutions, and actions
should be coordinated among these actors in order to solve the case. In case
of organ transplants there is an extra issue that is time: organs (such as heart,
lung, intestine, liver, pancreas, kidney) deteriorate rapidly between when they
become available and implantation (becoming useless in less than 6 hours in
some cases) – creating significant time pressure on transplantation. Furthermore
cases normally arise with a waiting list of patients waiting for a suitable
organ and a donation being made at a given moment in time meaning that the organ
then must be assigned to one of the waiting patients (or none if no good matches
are found). The activities of the individuals and organizations involved in
this case management are governed by several authorities during the transplantation
process. In particular the duty transplant surgeon takes initial responsibility
for coordinating the process, the Regional and national Authorities take charge
of assignment of organs to potential recipient and retrieval/implantation teams
manage the medical process of the actual operation (in most cases the same team
carries out both steps). A typical sequence in outline occurs as follows:
-
A donor becomes available.
The donor is assessed for potential donations by the duty transplant surgeon
and his/her team.
Data from medical records and these examinations is passed to the immunology
center to carry out potential matching tests and to the Organ Transplant Authority
to begin the search for a match.
After making a national check for extremely urgent cases, the OTA begins
a round robin process of all potential regional following established matching
criteria. Hospital with potential recipients in order decide whether or not
an organ could be assigned to one of their patients.
Immunology results are used to inform this process where available.
Once a decision is made, urgent arrangements are made for the recipient
to be contacted and prepared.
Medical procedure and accompanying logistics are prepared.
In most cases a team from the center at which the recipient will have the
organ implanted will travel to the center where the extraction will take place
to perform the extraction and subsequently return with the organ to the implantation
site.
The implantation surgery is followed by post care and monitoring of outcomes.
Provenance issues in OTM
As well as generic logging functions carried out by system components, the
OTM application requires more advanced analysis of the outcomes of organ transplantation
cases: both in terms of results generated by the software systems and in terms
of records of events which occurred in the real world. Requirements for analysis
come both from legal requirements (such as the Real Decreto 2070/1999/30th December:
regulating activities related to the procurement and clinical usage of human
organs and tissues and other Spanish law for systems to be deployed in Spain)
and clinical good practice. The following example provenance questions are a
sample of what would be of high value:
where did medical information used on each step of the process came from,
-
which medical actor was the source of information.
-
what kind of medical record was available to actors on each step of the
process
-
when a given medical process was carried out, and who was responsible for
it.
when a decision was taken, and what was the basis of the decision
which medical actors were asked to provide medical data for a decision
-
which medical actor refused to provide medical data for a decision
An example
To illustrate how provenance is handled in the OTM application, let us see
how the provenance of a medical decision is recorded and then queried. For that
we will select some few steps in a tipical transplant case. Let us consider
a patient who has previously given consent to donate his organs. As the patient’s
health declines and in foresight of a potential organ donation, one of the doctors
requests the full health record for the patient and then orders a serology test
through the OTM appli-cation. After brain death is observed and logged into
the system (along with the re-port certifying the brain death), if all requested
data and analysis results have been obtained, a doctor is asked to make a decision
about the patient being a potential donor. This decision is explained in a report
that is submitted as justification. The following figure shows a simplified
view fo this scenario, depicting the medical workflow that actors should follow
in this case.
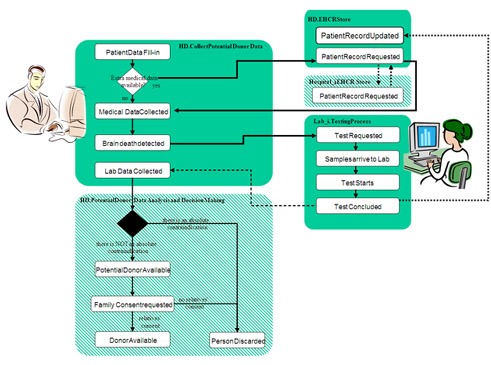
As OTM is a distributed system, the execution of the medical workflow is distributed
in different modules. Each module is responsible for monitoring parts of this
process, and record the relevant events and informations for a case. Coordination
and information sharing between these modules is achieved by message exchanges
among them. The following figure shows the messages exchanged by the different
modules of the OTM application in the same scenario.
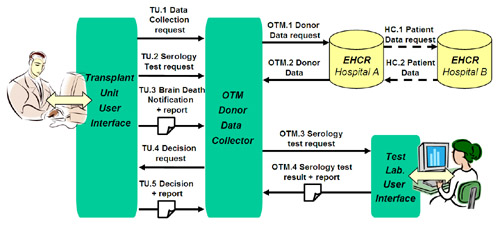
The Transplant Unit User Interface passes requests (TU.1, TU.2) to the OTM Donor
Data Collector service, which gets the electronic record from the EHCR system
(OTM.1, OTM.2). Sometimes all or parts of the record are not in the same insti-tution
but located in another institution (HC.1, HC.2). The Donor Data Collector service
also sends the request for a serology test to the laboratory and gets back the
result (OTM.4), along with a detailed report of the test. Reports are also passed
in the case of the Brain Death notification (TU.3) and the final decision report
(TU.5).
To make the OTM application provenance-aware, not only all interactions between
the different components of the system are recorded, but also the causal relationships
that link a given interaction with previous ones. This was done by modifying
the code of the OTM application to make explicit such relations. The following
figure gives an intuitive view of the effect of such relationship recording.
These explicit dependency relationships between interactions are the ones that
allow to create meaningful traces about the provenance of a given decision or
a given data item. We can see this by inspecting the documentation that OTM
would produce in such scenario. The figure below graphically represents the
subset of the p-assertions produced by the provenance-aware
OTM which are related to the donation decision. The part of the process that
happens within the electronic system is represented by interaction p-assertions
(regular boxes) for all interactions (TU.x, OTM.x, HC.x), and relationship
p-assertions (response_to, caused_by, based_on) capturing
dependencies between data. By making these dependencies explicit we can not
only connect different interactions but actually answer provenance question
by tracing back such dependencies.
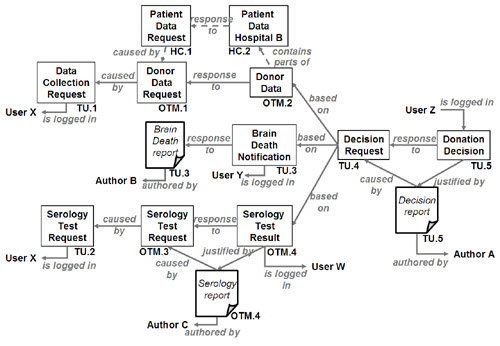
Even though what happens in the system has a parallelism to what happens in
the real world, this is not enough to fully answer which is the provenance of
a given decision. To solve this, the OTM system connects the documentation about
the electronic process to the real world by adding actor state p-assertions
stating who logged the information in the system (is_logged_in) and
when (not shown in picture), which are the reports that justify a given state
in the system (justified_by), who are the authors of these reports
(authored_by) and when the action reported was performed or the decision
taken (not shown). Following back the p-assertions graph in the above figure
OTM can trace the provenance of the donation decision (right-most box int he
figure), how it was based in some data and test requests, how a brain death
notification is also involved, who requested the information, where it came
from (in some cases it might come from the EHCR from another hospital), who
authored the justifying reports in the main steps of the process.
These provenance traces can be graphically represented to the users by means
of the provenance tools. Some of these tools also allow to do further analysis
over these traces. The following figure shows how the tool depitcs a provenance
trace for a donation case top the user.
During the process to make the OTM Application provenance-aware, we had to
find equilibrium between the amount of collected data and the level of interference
such data collection may cause in the real medical process. The use of the reports
and the information logged by the staff does not give full information about
what happens in real world, but gives more than enough information to trace
the individual or team involved, while not introducing an excessive increase
of work-load on the medical staff (we use the same reports medical staff already
produces). It is important to note that the person who is logged in might not
always be who authors the justifying reports (both are recorded in OTM), and
the time when things are re-ported to the system might not be the time when
things have happened (both also recorded in OTM). This is common practice in
medical teams: most of reporting is delegated to a team member having the proper
credentials and time to do it, although the report may be later checked and
even signed by a prominent member of the team.
Benefits of using provenance in OTM
By transforming OTM into a provenance-aware application,
we augment OTM with a capability to produce at run-time an explicit representation
of the process actually taking place;
such representation can be then queried and analysed in order to extract
valuable information to validate, e.g., the decisions taken in a given case,
or to make an audit of the system over a period of time.
